46 F with altered sensorium secondary to HIE
- Get link
- X
- Other Apps
Status epilepticus in a female with autoimmune diseases.
CHIEF COMPLAINTS:
She was brought with complaints of 2 episodes of involuntary movements of upper and lower limbs and hemoptysis in the morning.
HISTORY OF PRESENT ILLNESS :
She developed sudden onset movements of both upper and lower limbs at 5am in the morning which lasted for about 4-5mins , associated with confusion after the episode, without any trigger, aura .
she had an other similar episode while she was brought to the hospital.
She had similar episodes at the hospital.
SHE WAS APPARENTLY ASYMPTOMATIC 13 YEARS AGO,
Then she had low back ache and generalised weakness , for which she visited a local hospital.During the investigations, she was found to be having,?soft tissue overgrowth ,(as said by attenders ,no documentation)and need to get operated, during routine investigations creatinine was elevated, then she was started on conservative management .
(Tab Sodium bicarbonate,Shelcal,Omeprazole,Iron folate)
Since then ,she is on routine followup with hemogram and serum creatinine levels,and her baseline creatinine levels were maintained at 3.2mg/dL.
In june 2022,she developed fever and productive cough associated with SOB for which CT chest was done,showing peripheral ground glass opacities,and septal thickening .
Few days later , she developed swelling of both lower limbs till the level of ankles,which were insidious in onset and gradually progressive.
Then underwent dialysis for the first time through right IJV line,for 4 hours,and was on conservative management.
In September 2022, she developed fluid filled bleb, on one finger and then over all the 10 fingers of hand in 10 days ,some of which ruptured on their own and some were pricked by the patient.
She developed eroding nails and distorted nails , hyperpigmented macules over the face and itching over the palms,and low grade fever associated with loss of apetite and alopecia.
Ulcers over palms , pulp of fingers associated with burning sensation
With autoimmune etiology suspicion, she was investigated further
ANA profile was Positive for
Anti Ro 52
SSA/Ro 60++
SSB/La+.
In view of the persistent low Hb 5-6g/dL,bone marrow aspiration (from right posterior iliac spine)was done for evaluation of anemia.
Then she was started on mycophenolate mofetil 360mg,and later was planned to shift to cyclophosphamide as she is not responding to MMF.( But was not started in view of renal insufficiency).
SHE WAS PUT ON MYCOPHENALATE MOFETIL, HYDROXYCHLOROQUINE , OMNICORTIL .
In November she developed cough with whitish color sputum which is mucoid in consistency and moderate in amount and non blood stained and non foul smelling .
Bilateral swelling of lower limbs till knee,not associated with trauma,and decreased urine output for 2 days,and Shortness of breath( MMRC grade 3),and loss of appetite.
Then ,she was diagnosed as
*?Antisynthetase syndrome
*CLD secondary to autoimmune hepatitis with hypoalbuminemia *
acute exacerbation of ILD
*recurrent anemia
She did not develop any new skin lesions,oral ulcers.
In December,she was taken to another hospital
Due to increase in the SOB with abdominal distension ,
Then she was taken to second session of dialysis.
Her antibody profile was repeated.
Bronchoalveolar lavage was performed and was found to be having an infective etiology and mucus plugs in the airways.

On ultrasonography,hypoechoic lesions were found in the liver, PET CT was advised and was done.
So they suspected infective etiology probably TUBERCULOSIS,and started her on antitubercular therapy
Tab ISONIAZID 300mg daily
Tab RIFAMPICIN 500 mg OD daily
Tab PYRAZINAMIDE 1500 mg thrice a week
Tab ETHAMBUTOL 1200 mg thrice a week
on 15 th December .( But afb, genexpert are all negative)
CURRENT PRESENTATION
sudden onset movements of upper and lowerlimbs, for 3-4 minutes, associated with bleeding from mouth,with brief period of LOC .
similar episode one at 6:00 am, and then 2 similar episodes after they came here at 8:00am.
At presentation her blood pressure was 170/110 mmhg
inj lorazepam was given,
later leviteracetam and
when her seizures weren’t controlled then sodium valproate was given
She later then had continuous episodes of seizures lasting for more than 45 minutes .
In view of respiratory distress ( sats 60 ),and uncontrollable recurrent seizures she was sedated with IV MIDAZOLAM and intubated.
Post intubation, she had cardiac arrest ( no central pulses palpable ) 2 cycles of CPR done ROSC was achieved and post CPR monitor showed monomorphic VT and 2 times 200 J of DC shock was given and then it reverted to sinus tachycardia.
I examined her on day 2 at our hospital
GENERAL EXAMINATION
Patient is on sedation.
She has hyperpigmentation on the face, upper limbs
Her nails
Single Bleb on the right hand
VITALS:
Temperature:afebrile
BP 160/110mmhg
Pulse 158bpm
RR 37 cpm
SYSTEMIC EXAMINATION
CVS : S1,S2 heard. No murmurs
RS : Bilateral air entry present
Normal vesicular breath sounds were heard
CNS
Meningeal signs were absent
As the patient is sedated, I didn't elicit Sensory examination, Motor examination.
Pupils: mid dilated , reactive to light
DOLL'S EYE : present
Reflexes:
SUPERFICIAL:
CORNEAL REFLEX present
CONJUNCTIVAL REFLEX present
DEEP TENDON REFLEXES:
Rt. Lt
Biceps: 2+ 2+
Triceps 2+. 2+
Supinator. A. A
Knee. A. A
Ankle A. A
PROVISIONAL DIAGNOSIS:
STATUS EPILEPTICUS, seizures sec to
?autoimmune vasculitis
? Metabolic cause( increased urea)
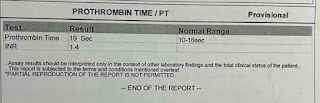
Investigations
ON DAY 1
She was maintained on ACMV MODE of ventilator
On day 9, tracheostomy was done and placed on SIMV mode
Weaning protocol was followed, from acmv shifted to cpap and then a trial of piece was done, but her RR was crossing 45 cpm, so she is currently maintained on cpap mode .
- Get link
- X
- Other Apps




























Comments
Post a Comment