A 32 YEAR OLD FEMALE WITH HYPOKALEMIC PARALYSIS WITH MULTIPLE JOINT PAINS
This is an online Elog book to discuss our patient deidentified health data shared after taking his/ her guardians sign informed consent
CONSENT AND DEIDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever
Cheif complaints :
Deformities of both hands since 1 year
Complaints of low grade fever since yesterday night.
Dry cough since yesterday night
HISTORY OF PRESENT ILLNESS:
A 32years old female,who is a daily wage labourer (stopped 1 year back),due to her deformity,came with complaints of deformities of bilateral hands and low grade fever and dry cough since yesterday night.
Patient was apparently asymptomatic 1 year ago,and then she developed mild deformity of right hand(ulnar deviation of fingers)second metacarpalophalengeal joint(initially to start with),not associated with any pain,redness and tenderness and the deformity sequentially progressed to 3rd,4th and 5th MCP in a period of 1 month.She initially thought her deformity is due to prolonged use of her hand in that position while working (plucking weed from field),and later after one month she developed similar sequence of deformity in other hand(left hand),2nd,3rd,4th and 5th MCP,in a sequence and then after 10 days she started developing pain in multiple joints (large and small of upper limbs and lower limbs)at same time and eventually after pain she developed swelling of all the involved joints not associated with any redness and local rise of temperature,and she developed swelling of her bilateral soles finding her unable to walk,with the above complaints she went to a local hospital for which she was given some medicine and used for 1 month and her pains subsided for that month,and later once she stopped those medication she again developed pains all over the joints,,and she has been abused by her husband these 7 months as she is not earning money,and sitting idle at home,and so she didn’t used medication for 7 months,and suffered from the same pain for 7 months and 15 days ago,she went to hospital again and was prescribed medication for which her pains got decreased now,and on sunday(3 days ago)at around 3am, while she felt some dragging sensation of the left lower limb she thought of pulling her legs close,but she couldn’t and she couldn’t raise her right upper limb,for which she pinched her left lower limb and right upperlimb herself and she didn’t felt any sensation and again,around 10am in the morning,she developed similar weakness in left upper limb and right lowerlimb and after an hour she couldn’t even hold her head,and for which she was taken to hospital around 2:00pm ,(her serum potassium was 1.65mEq/L)and was connected to Iv line(medication not known)and she regained her neck power initially(after 30 minutes) and after second infusion she regained power of left upperlimb and right lowerlimb and again after another infusion she regained power of right upperlimb and left lowerlimb and at 10:00am next day ,she regained her full power and she walked on her own,(serum potassium levels 6.8mEq/L) and she developed shortness of breath during the quadriparetic episode and decreased on its own,and she was referred to higher centre for management of hyperkalemia ,and patient came here for management and since yesterday she developed low grade fever with chills and dry cough and Sob on and off (since Sunday).
Restriction of mouth opening since yesterday and feeling of pain in the left cheek and zygomatic prominence when tried to open.
Early morning stiffness+
No deformity of wrist joint and no deformity of thumb.
No history of any nodules over body
Past History:
No similar complaints in the past.
History of dental implantation of upper 4 incisors,due to cosmetic appearance.
History of weight loss (8kgs)in 4years.
Not a known case of Dm,HTN,TB,Asthma,Epilepsy.
PERSONAL HISTORY:
Mixed diet,Normal apetite,Bowel and bladder moments regular,sleep adequate.
Treatment history:Using T.Hydrocholroquine 100mg tablets
MENSTRUAL HISTORY:
Cycles were regular,3/28 days.
She gave birth to 3 children(2 girls and 1 boy),by Cesarean section, each at a gap of 2 years starting from 20 years.
The age of last child(son)11years.
GENERAL EXAMINATION:
Patient is lean bulit and nourished.
Bilateral cervical lymphadenopathy +
Conjunctiva encroachment over eyes medial side in both eyes+
No pallor,icterus,cyanosis,clubbing,edema.
VITALS:
Bp:110/70mmHg
PR:84bpm
CVS: S1 and S2 Present
CNS:HMF intact
Patient is Afebrile at the time of presentation
No visible scars and sinuses .
JOINT EXAMINATION:
Bilateral 2nd,3rd,4th ,5th MCP of hands showing (ulnar deviation)deformity
Tenderness present over right 3rd PIP,and 2nd and 3rd MCP of right hand.
Thumbs of both hands are spared with no deformity.
Tenderness Present over bilateral temporomandibular joint,restriction of mouth opening +
No wrist joint deformity.
24hr urine protein is 195 sir,urinary creatinine 0.6,1300ml volume.Can we still consider SLE and send testing for immunological criteria sir??fever (constitutional domaina) and joint involvement +.atleast one clinical criteria is required and total of 10 points is needed
Chasing that diagnosis won't change our management plan currently
Did we get her echo? Please share the video.
https://www.nejm.org/doi/full/10.1056/NEJM196207052670103
Urine potassium15.6sir(25-125 mmol/lit is normal)🙆🏼♀️it came lower than normal sir😅
Check if it can come low in distal RTA
Yes sir I guess some problem with the recorders mobile @bhavana Intern ?will record it again and send
Urine anion gap in our patient is positive(228+15.6-221=26) indicating RTA in our patient
Gastrointestinal bicarbonate losses can be differentiated from RTA by estimating the urine anion gap. Negative urine anion gap indicates increased renal NH4 + production (extrarenal cause for metabolic acidosis), while positive gap suggests RTA
https://www.google.com/url?sa=t&source=web&rct=j&url=https://med.stanford.edu/content/dam/sm/pednephrology/documents/secure/1Renaltubdisorders.pdf&ved=2ahUKEwjs7cTxuoz6AhX6H7cAHU0nCTUQFnoECAcQBg&usg=AOvVaw0DGihPwaEYFM4SkGxaki6r
I am not finding urine potassium seperately being tested in dRTA sir.its urine anion gap they are referring to most of the times
Can you check what is normal Urine K+ range? Standardized values and not this lab value?
For adults, normal urine potassium values are generally 20 mEq/L in a random urine sample and 25 to 125 mEq per day in a 24 hour collection.
https://www.ucsfhealth.org/medical-tests/potassium-urine-test#:~:text=Normal%20Results,of%20potassium%20in%20your%20body.
DISCHARGE SUMMARY
Krishnamma
*Diagnosis*
Hypokalemia secondary to Distal renal tubular acidosis with autoimmune arthritis(? Jaccouds arthropathy? Rheumatoid arthritis)
TMJ arthritis
*Course in the hospital*
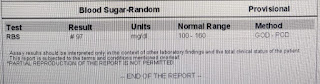
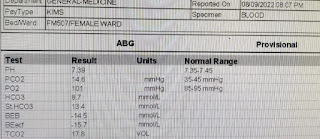
Patient was admitted with the above complaints and investigations were done showing mild hypokalemia,hyperchloremia,abg showing metabolic acidosis and urine ph:6,USG s/o left renal caliculi,24hr urine potassium 15.6(high/pseudonormal for the degree of hypokalemia) suggesting renal wasting of potassum:features suggestive of distal RTA
X rays s/o autoimmune arthritis?Jaccouds arthropathy? Rheumatoid arthritis .Keeping in mind the association of autoimmune disease (RA)and distal renal tubular acidosis patient is started on Tab Methotrexate 7.5mg once weekly,Tab Folic acid 5mg once weekly,Tab Nodosis 500mg BD,syrup potchlor 5ml+1glass water BD.Patient is adviced to regularly be in follow up with her serum potassium and bicarbonate values .OMFS (TMJ arthritis) and orthopedic referral was taken and advice followed
Advice at discharge
Tab methotrexate 7.5 mg OD weekly once on Fridays
Tab folic acid 5mg once daily every Saturday
Tab Nodosis 500mg PO TID
Syrup potchlor 5ml in 1glass water BD
Tab Flexon MR PO OD *2days
Cold fomentation of pre auricular area
Plan :Cementation of maxillary FDP
Hand surgeon opinion on Tuesday /Friday's for deformed MCP joints(in follow up with dept of orthopaedics)
OMFS review after 1 week in view of TMJ arthritis(In view of Cementation of maxillary FDP)
GM review on 15/9/2022 with serum electrolytes.











































Comments
Post a Comment